A 60-something woman complained of sudden severe abd pain. She was found by medics agitated, hypotensive, diaphoretic, and in shock.
There were 2 prehospital ECGs:
What do you think?
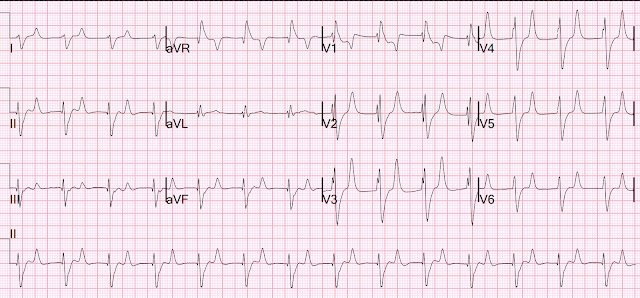
Smith: Uncertain supraventricular rhythm with PVCs. (See Ken Grauer's analysis below). There is "shark fin" in I and aVL, which is due to a combination of a large R-wave due to left anterior fascicular block plus downsloping ST elevation due to OMI. There is reciprocal STD in inferior leads. There is a rather large R-wave in lead V1 and a very large R-wave in V2, suggesting an atypical RBBB. There is huge ST depression across the precordial leads. There is STE in aVR. Thus, there is high lateral OMI with diffuse ST depression.
When I was shown this ECG, I said it looks like such widespread ischemia that is might be a left main occlusion, or LM ischemia plus circumflex occlusion (high lateral and posterior OMI). Moreover, left main occlusion often presents near death. In fact, most do not make it to the hospital alive, which explains why only a tiny percent of OMI are due to full LM occlusion.
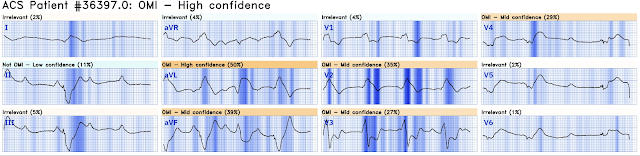
Here is the Queen of Hearts interpretation:
There is a second prehospital ECG:
 Again, supraventricular rhythm with RBBB and LAFB, shark fin, and STD maximal in V3. Posterior and high lateral OMI.
Again, supraventricular rhythm with RBBB and LAFB, shark fin, and STD maximal in V3. Posterior and high lateral OMI.But this time the Queen gets it wrong (thinks it is not OMI):
There were runs of VT:
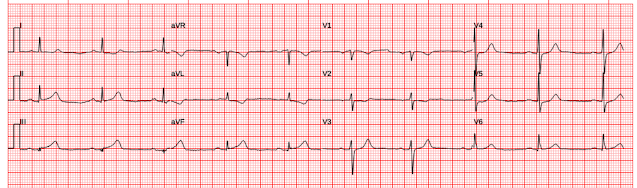
Tha patient arrived in profound shock and had an ED ECG:
Now there is some evolution to include the ST elevation (rather than ST depression) in V4-V6. This suggests that thrombus has propagated to occlude the LAD in addition to the circumflex.
It can be difficult to see ST elevation and depression when there is RBBB.
--It helps to find the end of the QRS.
--This is most easily done in lead V1.
--Then you can draw a line down through leads V2 and V3 to the lead II rhythm strip across the bottom.
--Then you can find the same location on the QRS in each 2.5 second interval.
--Then you can draw the line up to each of leads I, II, III; then aVR, aVL, aVF; then V4, V5,V6.
The Queen of Hearts gets it right here:
The interventionalist stated that he could not do the procedure while the patient has a blood pressure of 45 systolic.
Therefore, the patient was put on arterio-venous ECMO.
Then an angiogram was done.
There was a 100% Left Main Occlusion (OMI). It was opened and there was thrombus in the circ and LAD.
Unfortunately, the patient ultimately died.
Learning Points:
1. RBBB + LAFB in the setting of ACS is very bad. Some patients have baseline RBBB with LAFB, but in patients with likely ACS, these are associated with severe infarction with cardiac arrest, cardiogenic shock or impending shock.
2. Patients with ACS and RBBB/LAFB usually have a left main vs. proximal LAD.
Here are some cases of RBBB with LAFB:
3. Left Main Non-Occlusive ACS presents with widespread ST Depression and STE in aVR. Total Left Main Occlusion presents with different ECG findings which are multi-faceted.
See the variety of Left Main Occlusion ECGs here:
===================================
MY Comment, by KEN GRAUER, MD (5/3/2024):
===================================
Most patients with acute LMain Occlusion do not survive to make it to the hospital. Today's patient did make it to the hospital — but was in cardiogenic shock, and despite valiant attempt at treatment, succumbed soon after.
- I focus my comment on some additional Learning Points to those highlighted by Dr. Smith.
ECG Findings with Acute LMain Occlusion:
As per Dr. Smith — the ECG findings of total acute LMain occlusion are multifaceted. In Figure-1 — I reproduce major points that I've summarized from Dr. Smith's August 9, 2019 post on the subject. The KEY Take Home Points are as follows: - There is no “single” ECG presentation for patients with acute LMain occlusion. Quite literally — You can see almost anything!
- The reason for this highly variable ECG presentation, is that multiple territories may be involved to varying degrees — making it impossible to predict how much ST elevation you will see — and how much opposing (reciprocal) ST depression will attenuate (if not completely cancel out) these initial ST segment vector forces.
- The ST-T wave appearance in lead aVR can be anything when there is acute LMain occlusion.
 |
| Figure-1: Reasons for the varied ECG presentation of acute LMain occlusion — excerpted from Dr. Smith’s 8/9/2019 post (See text). |
"Shark Fin" ST Elevation and Depression
As per Dr. Smith — the 3 12-lead ECGs in today's case all showed prominent "Shark Fin" ST segment deviations.
- Dr. Smith illustrates in his discussion the delineation between the end of the QRS and the beginning of the ST segment for the 1st ECG done in the ED.
- For clarity in Figure-2 — I illustrate this delineation point for ECG #1 (ie, the 1st EMS ECG) — whereby everything to the right of the vertical RED lines that I've drawn in ECG #1 represents either marked ST elevation (in leads I,aVL and aVR) — or marked ST depression (in leads II,III,aVF; V1,V2,V3; V5,V6).
NOTE: For those wanting more practice recognizing Shark Fin ST-T wave changes — we've shown cases of this entity in the following ECG Blog posts (among others):
=====================================
What is the Rhythm in Today's Case?
Determination of the cardiac rhythm in today's case is of more than academic interest — since my initial "quick glance" of ECGs from this woman in her 60s who presented in shock — was that the QRS looked wide with an irregular rhythm that might represent a polymorphic VT.
- Looking closer — I recognized the Shark Fin morphology (that I illustrate with the vertical RED lines in ECG #1 of Figure-2).
How then to approach the rhythm in ECG-1?
- To Emphasize: I initially assessed the rhythm solely from ECG-1 — trying as I always to, "to put myself in the same position as providers in the field — who initially only saw ECG #1".
- As Dr. Smith has noted — recognition of Shark Fin morphology told us that the seemingly wide and irregular rhythm in Figure-1 was almost certain to be supraventricular!
- Despite the irregularity of QRS complexes — this rhythm is not AFib — because at least some definite P waves are present (RED arrows that I added at the bottom of ECG #1).
- Given that there are at least some definite P waves — I looked more carefully for spots in which more subtle signs of atrial activity might be present. I've labeled these places where I thought additional P waves are most probably present with PINK arrows.
- Taking yet another look — I have added WHITE arrows in places where I thought additional P waves might also be present (using simultaneously-recorded leads to assist in identifying probable P waves).
- BOTTOM Line: Realizing that there may be even more P waves than those that I labeled with colored arrows — I saw no way that the atrial rhythm was going to be regular. I also saw no PR intervals that repeated. Other than perhaps beats #13-thru-16, which looked regular — I thought there was no sign of sinus conduction. Other than knowing the rhythm was supraventricular and clearly irregular, but with lots of P waves with similar morphology (so that this was not MAT) — and with an extremely variable P-P interval — I simply wasn't sure how to define the rhythm. Some high-grade degree of AV block seemed to be present, but this still didn't explain how irregular the R-R interval was.
- Most of the time when there is complete AV dissociation (as there seemed to be here) — both P wave and QRS rhythms are at least fairly regular. But that did not appear to be the case here.
What ECG #3 Tells Us about the Rhythm:
As per my description above — I was uncertain in ECG #1 about the presence and nature of atrial activity — until — I saw ECG #3:
- RED arrows in the long lead II rhythm strip in ECG #3 — indicate P waves that I knew were present.
- PINK arrows indicate additional places where I thought there were subtle signs suggesting the presence underlying P waves.
- WHITE arrows indicate 3 places in the rhythm where although no sign of atrial activity was present — it could be easy to hide on-time P waves within the QRS complex of beat #7 — and within the ST-T wave of beats #10 and 11.
- BOTTOM Line: Unlike what I saw in ECG #1 — I thought the atrial rhythm in ECG #3 was regular. Other than a number of pauses (ie, before beat #1 — between beats #2-3 — and between beats #11-12) — the ventricular rhythm looked regular. That said — no PR intervals repeated, so once again I thought there was either high-grade or complete AV block. The different (upright) shape of the QRS for beat #4 suggested this might represent a PVC (or a fusion beat).
- In Retrospect: The fact that ECG #3 shows a series of definite P waves — is in strong support that the colored arrows I added to ECG #1 most likely do represent P waves, albeit with a fast and irregular atrial rate.
- Final Note: My insatiable appetite for collecting unusual arrhythmias spurred me in years past, to review of multiple continuous tracings from cardiac arrests in the hospital where I was Attending. Suffice it to say that, "The heart does whatever it will do when a patient is about to arrest". The "usual rules" of cardiac arrhythmias are simply not always followed in critically ill patients. Today's unfortunate case details a patient with acute LMain occlusion, that led to cardiogenic shock before her demise. This probably explains why the cardiac rhythms in Figure-2 defy classification.
-USE%20copy.png) |
| Figure-1: I've labeled the initial EMS ECG and the 1st 12-lead tracing done on arrival in the ED. |














-USE%20copy.png)


-USE.png)










.png)